Throughout our everyday lives, we consume large amounts of environmental proteins. In addition, our intestines have large populations of bacteria which can activate the immune system. To ensure the liver functions properly and to prevent dangerous inflammation, the immune system within the liver is appropriately suppressed.
When tumors develop in the liver, immunosuppression is amplified beyond what is physiologic, preventing patients from rejecting their cancer and responding to treatments.1,10
Specifically, the liver contains a high number of suppressive immune cells, of which certain subsets are expanded in the presence of cancer.2,3
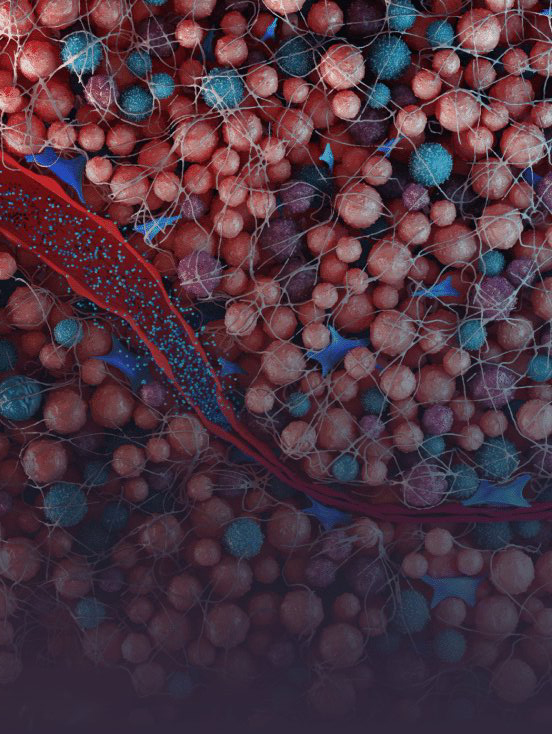
Throughout our everyday lives, we consume large amounts of environmental proteins. In addition, our intestines have large populations of bacteria which can activate the immune system. To ensure the liver functions properly and to prevent dangerous inflammation, the immune system within the liver is appropriately suppressed.
When tumors develop in the liver, immunosuppression is amplified beyond what is physiologic, preventing patients from rejecting their cancer and responding to treatments.4,10
Specifically, the liver contains a high number of suppressive immune cells, of which certain subsets are expanded in the presence of cancer.2,3
MDSCs are a heterogeneous population of immature myeloid cells that have the ability to suppress T-cell activity and responses to immunotherapy. Growth factors produced by the tumor promote MDSC proliferation and suppressive function.11,12
MDSCs produce nitric oxide, suppressive cytokines and reactive oxygen species to inhibit T cells through antigen-specific and nonspecific mechanisms. In addition to directly suppressing T cells, MDSCs promote angiogenesis, metastatic progression, and resistance to chemotherapy, targeted therapy, and immunotherapy.10,11
High levels of MDSCs enhance the tumor’s ability to drive increases in other suppressor cell populations.2
Primary liver tumors and liver metastases secrete growth factors that further expand the population of MDSCs. These cells have been shown to enhance the tumor’s ability to drive increases in other suppressor cell populations, such as regulatory T cells (Treg), and induce T-cell anergy.11
Higher MDSC infiltration correlates with poor overall survival (OS) and progression-free survival (PFS) in patients with solid tumors. It is believed that high levels of MDSCs enable a tumor to evade the immune system13–17 and generate further resistance to immunotherapy approaches such as checkpoint inhibitors and CAR-T therapeutics.4
Within the liver, MDSCs are programmed differently relative to other organs.11 This necessitates a tailored approach when developing immunotherapy regimens for patients with liver tumors.
Rapid tumor growth increases ITP and causes vascular collapse, impeding drugs from reaching higher-pressure regions within the tumor.18
Solid stress compresses blood vessels, which may reduce or halt blood flow to parts of the tumor.18 Tumor blood vessels are immature, leaky and disorganized, causing high interstitial pressure inside the tumor.18,19 In addition, solid stress leads to compressed lymphatic vessels, so pressure cannot be relieved by the lymphatic system.18-21
With traditional delivery approaches, these physical barriers often limit the uptake of therapy within the tumor.22 When drugs are delivered sub-optimally, the therapeutic index may be insufficient to achieve the desired clinical effect.
The liver tumor microenvironment is immunosuppressive due to an elevated level of MDSCs, while high ITP reduces the efficacy of drug delivery.22
At TriSalus, we believe a therapeutic approach that simultaneously reduces MDSC populations and improves therapeutic delivery to liver tumors and suppressive immune cells throughout the organ holds great promise for these patients that have few good options.
We encourage you to read and evaluate terms of use, privacy, security and other similar policies of the destination site as they may differ from TriSalus’ standards.
TriSalus assumes no responsibility nor does it control, endorse or guarantee any aspect of your use of any third party sites. Additionally, the presence of this link does not imply the third party site’s endorsement of TriSalus or this website.
Thank you for visiting our site.